by Adrian Glasser
This is a blog about a dynamic infrared pupillometer for real-time tracking and measurement of pupil diameter.
Often, clinically, pupil diameter is measured by a clinician by holding a ruler in front of the pupil of the eye of a patient to measure the pupil diameter to the nearest millimeter. This may be perfectly suitable for many clinical applications that require nothing more. However, today, with the advent of inexpensive USB video cameras, many with excellent infrared sensitivity, it is possible to do far more. One possible application, where more accurate and more detailed pupil diameter information might be required, is during near-vision testing. The ability of an eye to see near objects clearly, normally relies on an optical change in refracting power of the eye called accommodation. However, with aging and the onset of presbyopia, accommodation is progressively and ultimately completely lost by about age 55 years. However, the pupil of the eye continues to constrict when the eye makes an effort to focus at near even in the fully presbyopic eye. This near pupil constriction effectively increases the depth of focus of the eye which can aid distance corrected near vision in the presbyopic eye.
In this application, an infrared sensitive video camera with associated infrared LED is mounted on a spectacle frame to view the pupil of the eye at high magnification. The video camera and LED are controlled from software run on a laptop computer. The software allows for control of one or two LEDs. The LEDs can be turned on and off and the brightness adjusted. The live video image allows for the pupil to be tracked in real-time and the pupil diameter to be recorded. The data is accumulated and can be saved to a file for later analysis. In this way, the pupil diameter can be measured to a fraction of a millimeter and can be measured multiple times per second and can be recorded for long durations.
The video is best viewed by clicking on the full-screen icon at lower right on the video.
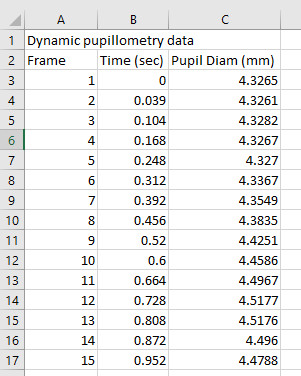
The software records the measurement number, the measurement time and the pupil diameter. At the end of a recording the recorded data can be saved to a file, such as in the image below, for later analysis. The analysis on this data can include the dynamics of the pupil response, such as to a flash of light, for example. With this approach, the pupil diameter could also be recorded as patients are performing an acuity task so that the pupil diameter can be known at the same time that the acuity is being measured.
An approach such as this could readily be implemented clinically to get more accurate and more useful information on the pupil diameter.
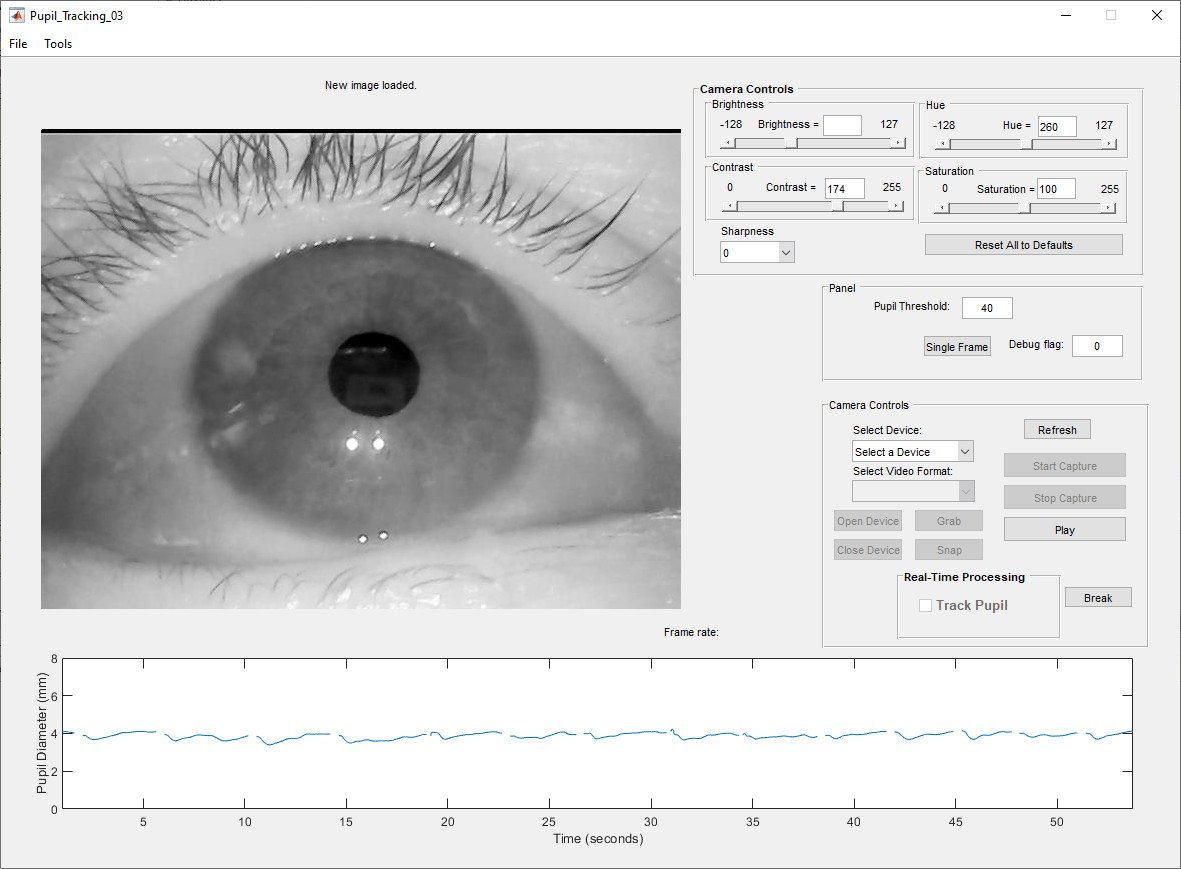
Here, below is an image of the software. In addition to allowing real-time pupil tracking and pupil diameter measurements, the software also allows image files and video to be saved, it allows image and video files to be loaded and allows the dynamically recorded pupil diameter data to be captured, saved and reloaded into the software to be graphed as shown.
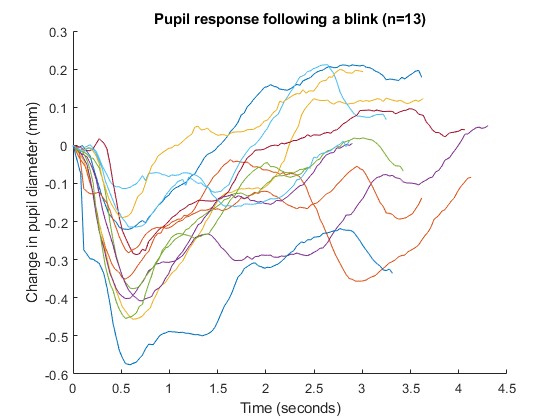
Below is an example of analysis of data collected (shown in the image above) with the dynamic pupillometer. The graph shows the change in pupil diameter that occurs after each blink. In the live recording of the pupil diameter, if a blink occurs, no data is collected for those time intervals in which the pupil is obscured by the eye lid. It is then straightforward to extract the pupil diameter data that is recorded immediately after a blink occurs. The graph shows how the pupil responds after 13 successive blinks. This data was collected in a darkened room, but with a single light on. As the eye lid opens after a blink, the pupil constricts to a minimum at about 600 milliseconds after the blink and then starts to dilate again over the following 2-3 seconds. This is an example of the kind of data that is available from a dynamic pupillometer and the kind of analysis that can be performed on such data.
A new, simplified graphic user interface has been developed. This facilitates the clinical deployment of the software.
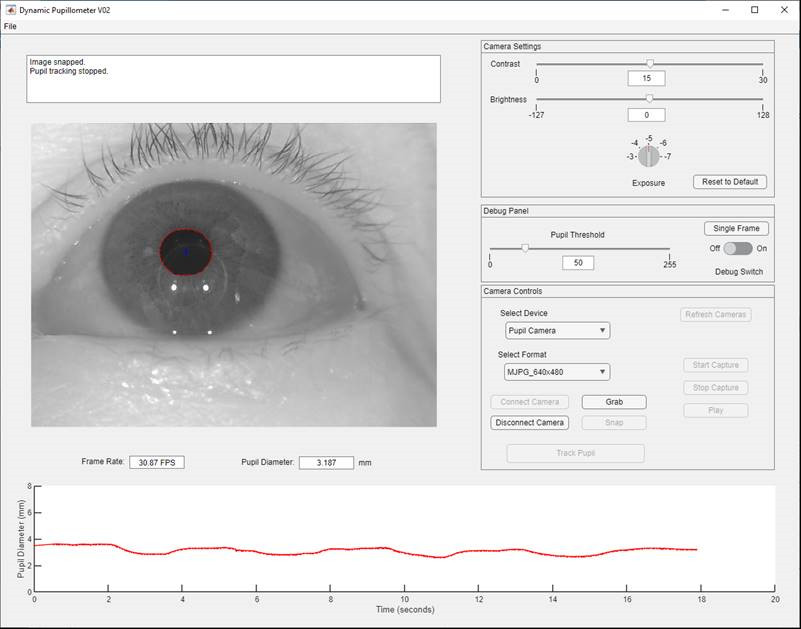
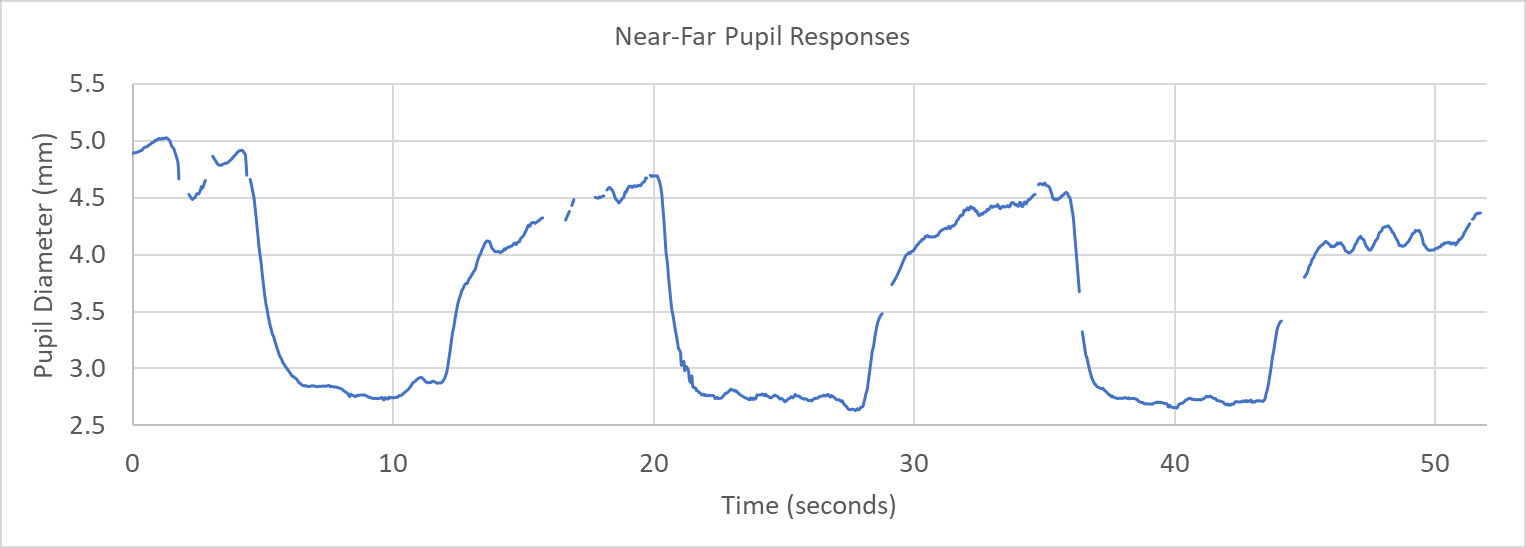
Here below is an example of the response of the pupil recorded during near and far viewing. The magnitude of the accommodative effort that is being exerted can be seen based on the pupil response recorded from a presbyopic eye making an effort to focus at near.
The ability to do dynamic pupillometry, to capture, save and analyze dynamically recorded pupil diameter data has many important clinical applications.